- Health
Time article on bone marrow transplant trial for multiple sclerosis treatment mostly accurate but needs more important details and context
Reviewed content

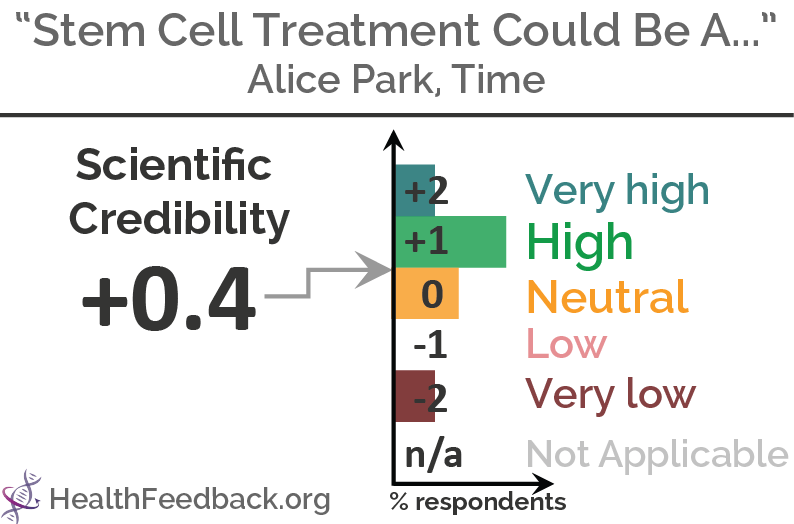
Headline: "Stem Cell Treatment Could Be A Game-Changer for MS Patients"
Published in Time, by Alice Park, on 2018-03-19.
Scientists’ Feedback
SUMMARY
This article by Time Magazine reports the preliminary results of a clinical trial for patients with multiple sclerosis (MS), a debilitating autoimmune disease that results in nerve damage. The trial found that bone marrow transplants (also known as hematopoietic stem cell transplant) led to fewer relapses in patients with a certain form of MS called relapsing MS, compared to patients who received standard therapy. These results suggest that bone marrow transplants are more likely to help MS patients live disease-free compared to current therapy.
Reviewers found the article to be generally accurate in summarising the main findings of the study, although mistakes in some crucial aspects were present. For instance, the sequence of events in the transplant procedure was described wrongly. Adding important details for clarity would have been useful, such as which group had conducted the trial and the type of stem cells used in the study (since many different types exist that are also used for treating other diseases). Providing additional context would also have better informed readers about the current state of knowledge about MS, such as the fact that the main causes of MS have been identified and that bone marrow transplants have already been used in several MS treatment studies prior to the one reported in the article.
You can read the original article here.
[This is part of a series of reviews of 2018’s most popular health and medicine stories on social media. This article has been shared more than 560,000 times.]
REVIEWERS’ OVERALL FEEDBACK:

Director, Mellen Center for Multiple Sclerosis Treatment and Research
Overall, the article is a reasonable summary of the study. One issue, however, is that the article never mentions the type of stem cell transplantation that was done. There are many types of stem cells and how they might be used. This study specifically tested immunoablation followed by hematopoietic stem cell transplantation (i.e. deleting the immune system with high-dose chemotherapy and regenerating it with a transplantation of blood-forming stem cells). The other points are: 1) the study has not yet been published and 2) the study had some methodological issues.

Director (CRPP Multiple Sclerosis), University Hospital Zurich
The article contains some inaccuracies and simplifications, but is overall accurate. It is not clear which article and whose scientific data it refers to. Such information should be mentioned in the article. The type of stem cells that were used for the procedure is also unclear.
Immune system renewal after hematopoietic stem cell transplantation has actually been demonstrated a long time ago by Muraro et al.[1] The article’s description of the procedure itself, i.e. the sequence of steps, is incorrect (see Annotations below for more details). Despite the clearly very promising results, it would have been good to state that the development of treatments for MS has been quite successful in the last two decades. Hematopoietic stem cell transplantation is clearly a step forward – although this is not yet accepted by many neurologists. However, it is an invasive treatment with a certain (albeit small) risk of dying from complications (mostly infections) during the period when the “old” immune system has been destroyed, and new immune cells are not yet reconstituted.
- 1 – Muraro et al. (2005) Thymic output generates a new and diverse TCR repertoire after autologous stem cell transplantation in multiple sclerosis patients. Journal of Experimental Medicine.

Senior Scientist (Neuroscience), Ottawa Hospital Research Institute
First of all, “stem cell treatments” are extremely sought after for treating many ailments and are a major source of medical tourism. The specific procedure being discussed in the article is a bone marrow transplant (BMT). Hematopoietic stem cells are used because without them, the chemotherapy given to destroy the malfunctioning immune system will also leave the body vulnerable (e.g. to infections) because it lacks sufficient white and red blood cells. There are other forms of stem cells – such as mesenchymal stem cells – that are being tested in MS that do NOT utilize chemotherapy[1,2,3].
Secondly, although this is the first truly randomized study of BMT in MS, there have been numerous other studies, some using other types of chemotherapy that have produced better results[4].
Finally, the target of MS is myelin, which is the insulation of the wires (not lining), which in the central nervous system is made by cells called oligodendrocytes. Although not all neurons require their wires (or axons as they are called) to be insulated in order to conduct, those that do usually convey the more important messages such as vision, motor capability, and sensation. It is believed that when the insulation is stripped away under attack from the faulty immune system, it exposes the underlying wire (axon) to the same inflammatory milieu and that ultimately leads to its destruction. Once there are no longer any wires, the neurons giving rise to those wires eventually succumb as well.
- 1 – Connick et al. (2012) Autologous mesenchymal stem cells for the treatment of secondary progressive multiple sclerosis: an open-label phase 2a proof-of-concept study. The Lancet Neurology.
- 2 – Cohen et al. (2017) Pilot trial of intravenous autologous culture-expanded mesenchymal stem cell transplantation in multiple sclerosis. Multiple Sclerosis Journal.
- 3 – Scolding et al. (2017) Cell-based therapeutic strategies for multiple sclerosis. Brain.
- 4 – Atkins et al. (2016) Immunoablation and autologous haemopoietic stem-cell transplantation for aggressive multiple sclerosis: a multicentre single-group phase 2 trial. The Lancet.

Senior Research Scientist, Tisch MS Research Center of New York
The article does not mention where the study was conducted or what drug it was compared to. They also don’t mention the side effects of the treatment, which can involve extended hospital stays. The article correctly points out that this may not be an appropriate approach for all patients with MS.

Professor, Careggi University Hospital
The article provides a good overview of the topic. However, a major misleading item needs to be addressed, which is the phrase “rebooting the immune system with healthy cells”, which suggests that stem cells from healthy donors are used. This is an autologous transplantation, therefore only the patient’s own stem cells are used (described in a review by Muraro et al.[1]; also see the figure below from the review for an overview of the procedure). It would have been better to phrase it as “rebooting the immune system with the patient’s own blood stem cells”.

- 1 – Muraro et al. (2017) Autologous haematopoietic stem cell transplantation for treatment of multiple sclerosis. Nature Reviews Neurology.

Cardiologist, Independent Expert
Overall a good article. The title contained some unfortunate buzzwords like “game changer” but the text itself fairly accurately reported on the results of the trial in question, mentioned limitations, and explained the context fairly well.
Annotations
The statements quoted below are from the article; comments are from the reviewers (and are lightly edited for clarity).
“Researchers reported encouraging results for a stem cell transplant for multiple sclerosis (MS) that some doctors and patients hope will be a breakthrough for MS treatment.“

Director (CRPP Multiple Sclerosis), University Hospital Zurich
“Stem cell transplant” should have been declared early on as “blood stem cell transplant” or “hematopoietic stem cell transplant”, to avoid confusion with all other stem cells that are used to “repair” organ damage, e.g. in the brain.
“People in the stem cell transplant group received chemotherapy to wipe out most of their current immune cells that were wrongly attacking neurons. They then took special medications to coax their stem cells, which produce the entire population of immune cells, out of the bone marrow and into the blood to start churning out new immune cells.“

Director (CRPP Multiple Sclerosis), University Hospital Zurich
It is actually the other way around: first comes the mobilization of blood stem cells from the bone marrow using special drugs, followed by the harvest of these cells from the peripheral blood. Finally, the chemotherapy is given to destroy immune cells.
“It’s not clear why the immune system in people with MS starts attacking its own nerve cells.“

Director (CRPP Multiple Sclerosis), University Hospital Zurich
There is now plenty of data showing that MS is a prototypic autoimmune disease with a complex genetic trait and a few environmental risk factors (e.g. Epstein-Barr virus, low levels of vitamin D, smoking, obesity) as main causes[1]. These factors lead to activation of pathogenic T and B cells, which then mediate the disease[2]. While there are certainly still open questions, the main causes have been identified.
- 1 – Olsson et al. (2017) Interactions between genetic, lifestyle and environmental risk factors for multiple sclerosis. Nature Reviews Neurology.
- 2 – Jelcic et al. (2018) Memory B Cells Activate Brain-Homing, Autoreactive CD4+ T Cells in Multiple Sclerosis. Cell.
“Some research suggests that genes, combined with exposures to environmental agents ranging from pollutants to chemicals in the diet, for example, could misdirect the immune cells to destroy neurons. Re-setting the system in people who develop the disease might erase those effects and give those with MS a chance at slowing or even beating their disease.“

Director (CRPP Multiple Sclerosis), University Hospital Zurich
Rather than erasing the effects of the genetic trait and exposure to the environmental factors, the proper explanation would be that the chemotherapy and hematopoietic stem cell transplant re-establish tolerance and halt the autoimmune process against brain tissue by eliminating disease-causing autoimmune T cells and rebuilding a new adaptive immune system.
“But the study is the first to rigorously test the stem cell transplant for MS.“

Director (CRPP Multiple Sclerosis), University Hospital Zurich
There have been several studies that tested this principle before. It is correct that this is the largest randomized controlled study of this kind.
“The transplants are also expensive, and people who need them would likely have to go to a specialized center and work with a team of transplant and neurology experts who are familiar with the technique.“

Director (CRPP Multiple Sclerosis), University Hospital Zurich
The cost of currently approved treatments are also high and surpass those of the hematopoietic stem cell transplant, which is a one-time treatment, after a few years.



